NEW PROVIDERS
Timothy Larkin, MD
Lahey Cardiology, Beverly
75 Herrick Street Suite 206
Beverly, MA 01915
(P) 978-927-8400 (F) 978-922-1452
Justin Martinez, MD
Lahey Institute of Urology, Beverly
75 Herrick Street Suite 219
Beverly, MA 01915
(P) 978-927-0714 (F) 978-927-9135
Mary McCaffrey, MD
Lahey Outpatient Clinic, Danvers
Gynecology Clinic
480 Maple Street Suite 103
Danvers, MA 01923
(P) 978-712-1400 (F) 978-712-1419
Mina Farahani, MD
Ophthalmology Consultants of Boston
107 Endicott Street Suite 303
Danvers, MA 01923
(P) 978-524-0050 (F) 978-524-0051
Laura Voicu, MD
Ophthalmology Consultants of Boston
107 Endicott Street Suite 303
Danvers, MA 01923
(P) 978-524-0050 (F) 978-524-0051
NEWS FROM NEPHO
SEPTEMBER 2019 EDITION
IN THIS ISSUE:
What information can I find on the NEPHO Website?
PRACTICE CHANGES/UPDATES
- Effective 9/9/2019, Garden City Pediatrics has transitioned to a new Electronic Medical Record system, E Clinical.
- Long time NEPHO member, Neil Mann, MD of the Center for Healthy Aging, passed away peacefully
at Beverly Hospital on September 5, 2019. Gloucester Times Obituary
SAVE THE DATE
NEW PHYSICIAN ORIENTATION
Date: October 24, 2019 @7:30 a.m.
Place: 500 Cummings Center – Suite 6500
Good Harbor Conference Room
Beverly, MA 01915
RSVP: Alycia.Messelaar@lahey.org or 978-236-1784
OPEN MEETING II
Place: Beverly Hospital Lecture Hall-Beverly, MA 01915
RSVP: Lisa.M.Driscoll@Lahey.org
For your convenience we will be conducting the same presentation at 3 sessions.
| THURSDAY OCTOBER 3 12:30 P.M. |
WEDNESDAY OCTOBER 9 7:00 A.M. |
TUESDAY OCTOBER 22 5:30 P.M. |
Video Conferencing is available for all meetings with the exception of October 9th @AGH.
Attendance at more than one Open Meeting will not provide additional attendance credit.
2019 PCP ATTENDANCE POLICY
2019 SCP ATTENDANCE POLICY
IPA / POD MEETINGS SUMMARY
Follow up
- Carol Freedman, RPh provided information on how practices can access inhaler instructional videos. There is a link on the NEPHO website under “Quick Links”. Additionally, the YouTube video for each inhaler can be searched by name. An EPIC smart phrase is being worked on.
- Liz Isaac shared a summary of the Rapid Meeting Assessments for the July and August POD and IPA. There was significant improvement across all questions; “topics covered” is an area of continuing opportunity.
- Dr. Joe Peppe reviewed detail regarding Medicare ACO nationwide experience, minimum threshold for downside risk, timeline for entering a downside contract, and whether there is an opt out.
Reporting
- The Quarter 1 2019 PCP Report Card was presented to September PODS with discussion of key changes.
- Updated attendance through August meetings was shared.
Pharmacy
- Carol Freedman reviewed an education program that is being developed for management of diabetes consistent with current ADA guidelines.
- Topics include: key takeaways from 2019 guideline updates; benefits of newer agents; and quick pearls for general diabetes management including, but not limited to expected A1c reduction and appropriate medication adjustment intervals.
Quality
- Liz Isaac shared an update on Cervical Cancer Screening Performance year to date, reviewed ongoing initiatives, and invited discussion on ways to improve performance on this measure.
- Updated Quality AQC Action Lists and Scorecards were distributed.
Patient Experience
- Updated star ratings for timeframe January 2018 through June 2019 were distributed at POD meetings along with patient feedback.
- The plan is to post star ratings and comments beginning in fall.
Informational
- A new process for meeting reminder emails was shared. There will be two emails sent with agenda for upcoming month of meetings, as well as a listing of all the meetings that will be held so that providers can choose to attend another meeting in the event of a conflict.
- Logistics regarding the upcoming NP/PA meeting in September were shared.
PAYOR UPDATES
Commonwealth Care Alliance
Commonwealth Care Alliance (CCA) is partnering with a new vendor, Performant Recovery, Inc. to review provider claims. Performant offers claim review services that include the identification and resolution of underpayments and overpayments due to erroneous claims coding and/or incorrect claim adjudication.
If a need to review claims is identified by Performant, it is important that CCA providers follow instructions in the Performant letters requesting medical records. Performant will follow these timelines in the letter based on CCA’s guidance. Providers who do not follow the instructions risk the possibility of claims being retracted for “non-response”, as this is considered an agreement with the review findings.
Throughout an actual review process, Performant will offer specialized support. If you have any questions, please contact CCA Provider Services at (866) 610-2273.
Harvard Pilgrim Healthcare
Provider Directory Updates: CAQH Direct Assure Process Launched
Harvard Pilgrim, in collaboration with HealthCare Administrative Solutions, has begun piloting CAQH’s DirectAssure® with a user group of providers.
This approach will enable providers to update their demographic and practice information in one place and share it simultaneously with multiple health plans. Because DirectAssure® works in concert with CAQH ProView, an online database that most providers already use to regularly review and attest to professional and practice information, this approach capitalizes on an existing workflow and will streamline the process of keeping directory information up to date.
Phased in approach
We are phasing in implementation to support a smooth roll out of this functionality. This tool was successfully piloted in August with a small group of providers and will be rolled out more broadly to several hundred providers in September. To date, we are focused on roll out to providers who directly contract with Harvard Pilgrim, rather than those who are participate in large provider organizations as CAQH is working on developing functionality to best support more complex provider entities.
Pilot users will provide feedback on the system, and we will be working together to confirm that any updates submitted are received and listed accurately in the provider directory.
We will continue to roll this out to other providers in the coming months and will provide additional information about the next phases in future issues of the newsletter.
For more information about the DirectAssure® project, please refer to these resources:
Updating directory information if you aren’t a pilot user
If you are not part of the initial rollout of DirectAssure®, continue to use existing processes to review and report changes to your address, panel status (open or closed) for each individual provider, institutional affiliations, phone number, and other practice data. Please review this information at least quarterly to ensure that patients have access to accurate information to help them in selecting and contacting providers for care.
Notification of address, panel status, and other demographic information changes should be submitted at least 30 days in advance. You may review your practice information via our online Provider Directory. If you need to update any information, please fill out a Provider Change Form and submit it to NEPHO by email at Janelle.N.Jensen@Lahey.org or Alycia.Messelaar@Lahey.org.
For any further quesmailto:PPC@harvardpilgrim.orgtions, call the commercial Provider Service Center at 800-708-4414 or the Medicare Advantage Provider Service Center at 888-609-0692.
PROVIDER RELATIONS
Thank you to all of you who joined us for the NEPHO Office Manager meeting on September 11, 2019.
Special thanks to Ashley Gleason of Lahey Primary Care, Beverly and Maria Valliere of Lahey Primary Care, Danvers, for sharing their best practices for driving EPIC Best Practice Advisory response rates!
For those of you who were unable to attend, CLICK HERE to view the presentation. If you have any questions, concerns or ideas for future presentations, please reach out to Alycia Messelaar 978-236-1784 or Alycia.Messelaar@lahey.org .
 Stephanie Cunningham presents Best Practice Advisories in EPIC
Stephanie Cunningham presents Best Practice Advisories in EPIC
at September Office Manager meeting
QUALITY
A Little Hypertension R & R
As we head into the final months of the 2019 Blue Cross Quality Measurement Period, we as a PHO need to get 54 more compliant diabetic BPs and 141 more compliant hypertensive BPs to reach the maximum thresholds in both measures. The target values for both blood pressure measures are the same:
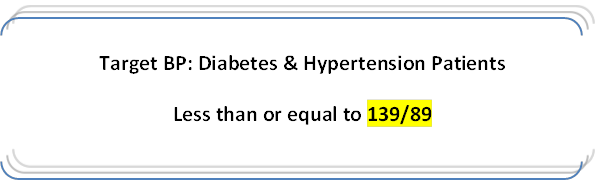
To help us achieve these goals, we need a little R & R: Retake and Reschedule.
- Retake an over target BP at some point during the encounter.
- Repeating a BP slightly over target will often bring it into the compliant range.
- Blood pressure measuring gurus: Please do NOT round up!
- Blue Cross will accept a composite BP that is compliant – see the example below
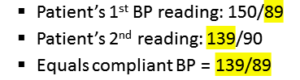
Reschedule the patient for a follow-up visit or BP check ideally by November 1st.
- If after 2 or 3 tries the blood pressure is still elevated, reschedule the patient for another appointment by 11/1/19.
- There does not need to be a claim for an office visit for the BP to count, so consider a BP check with an MA or RN and record the BP in the chart.
The LAST blood pressure of the year taken by a provider managing the patient’s diabetes or hypertension is the one that is submitted to Blue Cross. This can be taken by the PCP, an Endocrinologist, Cardiologist or Nephrologist if they are involved in managing the patient’s hypertension. Our PHO staff also emails and flags these specialists to alert them to upcoming appointments and remind them to pay attention to blood pressure readings.
Have questions? Need your updated patient list? Jennifer Andersen jennifer.s.andersen@lahey.org 978-236-1747, Laureen Viel, laureen.viel@lahey.org 978-236-1746.
PHARMACY UPDATES
Pharmacy – Pneumococcal Vaccination in Adults
See Pneumococcal Vaccination in Adults: Who Gets What and When? For more details.
- 2014 guidelines for immunocompetent adults 65 and older recommended giving Prevnar 13 followed by Pneumovax 23 one year later with a goal of decreasing pneumococcal infection rates.
- NEW CDC guidelines, soon to be released, are expected to change for seniors who are mainly protected from strains in Prevnar 13 by “herd immunity”, due to successful vaccination of children.
- Expect updated CDC recommendations to advise “shared clinical decision-making” with seniors when considering Prevnar 13.
- Prevnar 13 prevents just 1 case of outpatient pneumonia for every 2,600 healthy seniors immunized per year and giving Prevnar 13 to healthy seniors only prevents 1 case of invasive pneumococcal disease for every 26,300 immunized per year.
- Prevnar 13 costs about $190/dose.
- Focus on giving Pneumovax 23 to seniors 65 and older. It protects against 11 serotypes not covered by herd immunity from Prevnar 13.
- For now, when healthy seniors choose to get both vaccines, continue to give Prevnar 13…then Pneumovax 23 one year later. Medicare Part B still covers both if they’re spaced at least one year apart.
- Advise that immunocompromised adults (chronic renal failure, etc) of any age get both vaccines. Give Prevnar 13, then Pneumovax 23 at least 8 weeks later…to limit unprotected time in these more vulnerable patients.
- Continue to recommend Pneumovax 23 for adults UNDER 65 who smoke or have chronic conditions…and Prevnar 13 as a routine vaccine in kids.
Reference:
Clinical Resource, Pneumococcal Vaccination in Adults: Who Gets What and When? Pharmacist’s Letter/Prescriber’s Letter. September 2019.
For questions or more information contact Carol Freedman, NEPHO Pharmacy Manager 978 236 1774 OR carol.freedman@lahey.org
Proposed Policy, Payment, and Quality Provisions Changes to the Medicare Physician Fee Schedule for Calendar Year 2020
On July 29, 2019, the Centers for Medicare & Medicaid Services (CMS) issued a proposed rule that includes proposals to update payment policies, payment rates, and quality provisions for services furnished under the Medicare Physician Fee Schedule (PFS) on or after January 1, 2020. The proposed rules will be announced sometime in November 2019.
The calendar year (CY) 2020 PFS proposed rule is one of several proposed rules that reflect a broader Administration-wide strategy to create a healthcare system that results in better accessibility, quality, affordability, empowerment, and innovation.
Background on the Physician Fee Schedule
Payment is made under the PFS for services furnished by physicians and other practitioners in all sites of service. These services include, but are not limited to, visits, surgical procedures, diagnostic tests, therapy services, and specified preventive services.
In addition to physicians, payment is made under the PFS to a variety of practitioners and entities, including nurse practitioners, physician assistants, and physical therapists, as well as radiation therapy centers and independent diagnostic testing facilities.
Payments are based on the relative resources typically used to furnish the service. Relative Value Units (RVUs) are applied to each service for physician work, practice expense, and malpractice. These RVUs become payment rates through the application of a conversion factor. Payment rates are calculated to include an overall payment update specified by statute.
PAYMENT PROVISIONS
CY 2020 PFS Rate setting and Conversion Factor
CMS is proposing a series of standard technical proposals involving practice expense, including the implementation of the second year of the market-based supply and equipment pricing update, and standard rate setting refinements to update premium data involving malpractice expense and geographic practice cost indices (GPCIs).
With the budget neutrality adjustment to account for changes in RVUs, as required by law, the proposed CY 2020 PFS conversion factor is $36.09, a slight increase above the CY 2019 PFS conversion factor of $36.04.
Medicare Telehealth Services
For CY 2020, CMS is adding the following codes to the list of telehealth services: HCPCS codes GYYY1, GYYY2, and GYYY3, which describe a bundled episode of care for treatment of opioid use disorders.
Payment for Evaluation and Management (E/M) Services
Consistent with goals of burden reduction, CMS is proposing to align E/M coding with changes laid out by the CPT Editorial Panel for office/outpatient E/M visits. The CPT coding changes retain 5 levels of coding for established patients, reduce the number of levels to 4 for office/outpatient E/M visits for new patients, and revise the code definitions. The CPT changes also revise the times and medical decision making process for all of the codes, and requires performance of history and exam only as medically appropriate. The CPT code changes also allow clinicians to choose the E/M visit level based on either medical decision making or time.
Physician Supervision Requirements for Physician Assistants (PAs)
CMS is proposing to modify the regulation on physician supervision of PAs to give PAs greater flexibility to practice more broadly in the current health care system in accordance with state law and state scope of practice. In the absence of State law governing physician supervision of PA services, the physician supervision required by Medicare for PA services would be evidenced by documentation in the medical record of the PA’s approach to working with physicians in furnishing their services.
To reduce burden, of re-documentation CMS is proposing broad modifications to the documentation policy so that physicians, physician assistants, nurse practitioners, clinical nurse specialists, and certified nurse-midwives could review and verify (sign and date), rather than re-documenting, notes made in the medical record by other physicians, residents, nurses, students, or other members of the medical team.
Care Management Services
CMS is proposing to increase payment for Transitional Care Management (TCM), which is a care management service provided to beneficiaries after discharge from an inpatient stay or certain outpatient stays.
Another proposal includes a set of Medicare-developed HCPCS G codes for certain Chronic Care Management (CCM) services. CCM is a service for providing care coordination and management services to beneficiaries with multiple chronic conditions over a calendar month service period. CMS is proposing to replace a number of the CCM codes with Medicare-specific codes to allow clinicians to bill incrementally to reflect additional time and resources required in certain cases and better distinguish complexity of illness as measured by time. CMS is also proposing to adjust certain billing requirements and elements of the care planning services. These changes would also reduce burden associated with billing the complex CCM codes.
Recognizing that clinicians across all specialties manage the care of beneficiaries with chronic conditions, CMS is also proposing to create new coding for Principal Care Management (PCM) services, which would pay clinicians for providing care management for patients with a single serious and high risk condition.
Medicare Coverage for Opioid Use Disorder Treatment Services Furnished by Opioid Treatment Programs (OTPs)
Section 2005 of the Substance Use–Disorder Prevention that Promotes Opioid Recovery and Treatment for Patients and Communities (SUPPORT) Act established a new Medicare Part B benefit for opioid use disorder (OUD) treatment services, including medications for medication-assisted treatment (MAT), furnished by opioid treatment programs (OTPs). To meet this statutory requirement, CMS is specifically proposing:
- Definitions of OTP and OUD treatment services
- Enrollment policies for OTPs
- Methodology and estimated bundled payment rates for OTPs that vary by the medication used to treat OUD and service intensity, and by full and partial weeks
- Adjustments to the bundled payments rates for geography and annual updates
- Flexibility to deliver the counseling and therapy services described in the bundled payments via two-way interactive audio-video communication technology as clinically appropriate
- Zero beneficiary copayment for a time limited duration
CMS intends to implement this benefit beginning January 1, 2020, as required by the SUPPORT Act.
CMS is proposing to create new coding and payment for a bundled episode of care for management and counseling for OUD. The new proposed codes describe a monthly bundle of services for the treatment of OUD that includes overall management, care coordination, individual and group psychotherapy, and substance use counseling. One code describes the initial month of treatment, which would include administering assessments and developing a treatment plan; another code describes subsequent months of treatment; and an add-on code describes additional counseling. CMS is proposing that the individual psychotherapy, group psychotherapy, and substance use counseling included in these codes could be furnished as Medicare telehealth services using communication technology as clinically appropriate.
Please contact Shawn Bromley at shawn.m.bromley@lahey.org or 978-236-1704 if you have questions Medicare proposed changes coming in 2020 and 2021.
PATIENT EXPERIENCE COMMENTS
Cape Ann Pediatrics – 298 Washington Street, Gloucester, MA
• Dr. Thomas Carbone was very kind and compassionate.
Lahey Primary Care, Beverly – 900 Cummings Center
• Dr. Andrew Lenhardt is the best doctor I have ever had and the office runs smoothly.
Lahey Primary Care, Beverly – 30 Tozer Road
• Dr. Gail Ellisis wonderful, kind and compassionate.
• Dr. Tina Waugh has been excellent to all my medical needs, she is the best.
Lahey Primary Care, Danvers – 5 Federal Street
• Dr. Mauri Cohen the best ever!
Lahey Primary Care, Danvers – 480 Maple Street
• Dr. Galina Feldman is the best primary care physician I have ever had! Honest and knowledgeable.
Lahey Primary Care, Gloucester– 298 Washington Street
• Dr. Victor Carabba is extremely knowledgeable, kind and caring. I strongly recommend him.
Lahey Primary Care, Hamilton – 12 Railroad Avenue
• Dr. Laurence Gordon is wonderful. I have recommended him to family members. He really cares.
Lahey Primary Care, Manchester– 195 School Street
• Dr. Jana Oettinger is fabulous. Best PCP ever!
• Dr. Nicholas Avgerinos is the best. Spent so much time with me and he is so compassionate.
Thomas Pearce, MD – 279 E Main Street, Gloucester, MA
• Dr. Thomas Pearce listens and is concerned. I am always at ease.
Patton Park Medical – 42 Asbury Street, South Hamilton, MA
• I have been with Dr. Michael Edwards for 38 years and have no plans to leave him!
PRACTICE RECOGNITION
The Northeast PHO recognizes colleagues who provide a positive experience for our patients, help us keep care local and meet our quality targets.
This month’s winners are:
Dianetti Jimenez, Lahey Primary Care – Danvers, was recognized for her outstanding patient comment: “Ms. Jimenez in the lab is the BEST”
Kelley Moore, North Shore ENT, was recognized for her efforts to keep specialty care in the Northeast PHO network.
Please let us know if you have any office staff you would like to nominate for the recognition program.
We appreciate their efforts in supporting the PHO goal to provide high quality, community health care. We will deliver gift cards to the winners each month, and they will be announced here in the newsletter.
Be sure to look for the new winners in next month’s issue!