NECoMG Annual Meeting
Click here to read Dr. Sebba’s bio and the bios of this year’s Board of Directors candidates.
NEW PROVIDERS
No new providers at this time. Check back next month.
PRACTICE CHANGES / UPDATES
Steven Keenholtz, MD of Lahey Health Primary Care, Danvers will be retiring effective June 30, 2021. Please click here to read a wonderful article about Dr. Keenholtz being honored for his service and see below for a retirement memo from Dr. Keenholtz.
NEWS FROM NEPHO
MAY 2021 EDITION
IN THIS ISSUE:
Retirement Message from Steven Keenholtz, MD
BILH Guidance on Masking, Physical Distancing and Permitted Personnel (as of 6/1/21)
RETIREMENT MESSAGE FROM STEVEN KEENHOLTZ, MD
 It is with some sadness and a great deal of pride that I am announcing my retirement effective June 30, 2021. I have been a member of the Beverly Hospital medical staff since 1971. When I started in practice there were no Infectious Disease specialists on the medical staff at Beverly Hospital and 2 local municipal hospitals. After 2 1/2 years in a group, I opened a practice in Danvers providing both primary care and consultative Infectious Diseases services.
It is with some sadness and a great deal of pride that I am announcing my retirement effective June 30, 2021. I have been a member of the Beverly Hospital medical staff since 1971. When I started in practice there were no Infectious Disease specialists on the medical staff at Beverly Hospital and 2 local municipal hospitals. After 2 1/2 years in a group, I opened a practice in Danvers providing both primary care and consultative Infectious Diseases services.
I began practicing shortly after the first cases of HIV/AIDS were reported. I embraced the ability to provide high quality integrated care to patients at a time when there was no effective therapy for individuals suffering from HIV and dying at alarming rates. In 1985 the first of what would be many medications became available to treat HIV (AZT). In 1997 the first HIV cocktails transformed a uniformly fatal disease into a chronic infection. In addition, I provided support for those living with or affected by HIV as both a medical consultant and board member of Strongest Link Aids Services. Strongest Link is now part of the Aids Action Committee.
In 1983 I started “The Travel Clinic” which provided immunizations, prescription medications and counseling services for the greater North Shore communities. Over the years I have serviced thousands of individuals and groups including both pleasure and business travelers, mission groups, and school groups. We also provided immunizations for occupational risk groups including veterinarians, dentists, and animal control officers. Although the Covid-19 pandemic has radically altered people’s ability to travel it is expected that the service will continue as a part of North Shore Primary Care and Travel Clinic.
In addition to caring for HIV and providing preventative services for travel, I was the sole provider of consultative services for inpatient and outpatients needing infectious disease expertise. I remained the only ID specialist until I recruited Lucas Wolf to our community. I also served as the chairman of infection control until 2008 when I elected to focus primarily on outpatient medicine.
In addition to my subspecialty, I was a primary care provider to one of the larger panels in the community. I embraced the role of advanced practitioners and provided supervision to both nurse practitioners and physician’s assistants. Some of my patients have been under my care for as long as 40 years.
2020 presented transformative changes to medical practice due to the Covid-19 pandemic. During the initial surge I provided telehealth for 4 months until our office reopened in July. I have embraced returning to face to face medical care. I have also been a member of the Safety Committee for the Beth Israel Lahey Health Primary Care network helping develop the protocols to continue to practice safely despite Covid’s resurgence.
I am honored to have been an integral part of the Beverly Hospital community and to have earned the trust of both patients and colleagues. I look forward to spending more time with my wife Roberta, 3 children and 6 grandchildren. I will also continue to pursue my many hobbies including skiing, running, gardening, cooking, and fishing. Hopefully 2021 will allow us to be together so I can say farewell in person.
SAVE THE DATE
Date: Wednesday, June 16, 2021 @11:30am – 12:30pm
Coding Diabetes with Complications Overview
Location: GoogleMeet Conference Call
RSVP: Margaret.M.Doyon@Lahey.org
Date: Wednesday, July 14, 2021 @11:30am–12:30pm
Coding and Billing – Sneak Peek at 2022
Location: GoogleMeet Conference Call
RSVP: Margaret.M.Doyon@Lahey.org
Date: Wednesday, August 11, 2021 @11:30am–12:30pm
ICD-11 Overview
Location: GoogleMeet Conference Call
RSVP: Margaret.M.Doyon@Lahey.org
NEW PHYSICIAN ORIENTATION
Date: Tuesday, June 22 @ 5:30 pm
Location: GoogleMeet Conference Call
RSVP: Alycia.Messelaar@Lahey.org or 978-236-1784
Date: Wednesday, September 8, 2021 @11:30am–12:30pm
Coding and Billing Webinar: TBD
Location: GoogleMeet Conference Call
RSVP: Margaret.M.Doyon@Lahey.org
BILH GUIDANCE (as of 6/1/21)
As vaccination rates continue to rise and the impact of COVID-19 lessens in Massachusetts, masking requirements are relaxing in the community setting. Accordingly, BILH is updating our masking and physical distancing requirements for vaccinated personnel in certain circumstances.
Masking
Effective June 1, we are ending masking requirements for vaccinated staff in non-patient facing settings (see definitions below) in accordance with the state’s updated mask requirements that go into effect Saturday, May 29, and recommendations from the Centers for Disease Control and Prevention’s (CDC).
Given that we care for immunocompromised patients who may be at high risk of acquiring COVID-19, even if they are vaccinated themselves, we will continue to require masking in patient-facing areas, regardless of an employee’s or a patient’s vaccination status.
BILH encourages all staff who have not yet been fully vaccinated to do so for their own protection and that of their patients and colleagues. All BILH staff can walk in to BILH COVID-19 vaccination clinics – no appointment is necessary and individuals do not need to be a patient of BILH.
Highlights of the new guidance are in the table below. All guidance goes into effect at all BILH hospitals and business units on Monday, June 1. You can read the full guidance – Interim BILH Masking and Physical Distancing Guidance for Healthcare Personnel, Patients and Visitors and Interim Guidance on Return of Students, Volunteers and non-BILH Personnel – on the BILH COVID-19 website.
BILH Requirements for Masking for Healthcare Personnel (as of 6/1/21)

Please note the following important information:
- If a vaccinated individual is uncomfortable removing their mask while not knowing the vaccination status of all individuals present, they can still wear a mask.
- All staff – vaccinated and unvaccinated – must continue to perform daily symptom reportingbefore reporting to a BILH facility for work.
See full guideline for information on patient, visitor and essential escort masking.
Physical Distancing
- Physical distancing is no longer required for vaccinated or masked unvaccinated staff.
- Vaccinated staff do not require physical distancing in staff-only spaces to eat or drink.
- Unvaccinated staff should maintain physical distancing when unmasked to eat or drink.
Expansion of Non-BILH Personnel
BILH has also updated its Interim Guidance on Return of Students, Volunteers and non-BILH Personnel to include:
- One observer at a time is now permitted in clinical areas.
- Students and volunteers ages 14-18 are now permitted on campus.
- Vendors are permitted on site for patient care, training and essential infrastructure work.
- Hiring interviews may be conducted virtually or in-person at the discretion of Human Resources.
Thank you for your ongoing commitment to keeping our patients, their families and our colleagues safe.
PAYOR UPDATES
Blue Cross Blue Shield of Massachusetts
Authorization Requirements by Products
BCBSMA has posted an updated Authorization Requirements by Products. To view the complete list, click here.
Harvard Pilgrim Health Care
Complex Case Management Services
These programs assist patients with conditions such as chronic kidney disease, cancer, heart disease, asthma, diabetes, and a variety of rare diseases. Complex case managers help patients avert the need for more intensive medical services by providing them with information tailored to their needs and stage of readiness. The case management programs proactively identify at-risk patients, who typically have co-morbidities and psychosocial needs that can significantly diminish their quality of life and make it difficult for them to adhere to treatment plans. Case management programs are available to members identified through: 1) Algorithms based on medical, pharmacy, and/or radiology claim analysis, 2) Hospital discharge data, 3) Provider and case manager referral, 4) Self-referral, 5) Health risk appraisal. For additional information and to view the notification, click here.
Tufts Health Plans
Nurse Practitioner and Physician Assistant Professional Payment Policy Update
Reviewed by committee; added Tufts Health Public Plans content to combine policies; clarified billing and compensation information. To view the complete policy, click here.
PROVIDER RELATIONS

Please click here to take a moment to read the Provider Spotlight on Dr. Richard Peinhart of Howard Goldberg, MD, Inc.
If you would like to be featured on the PHO website, please reach out to Alycia Messelaar Alycia.Messelaar@Lahey.org or 978-236-1784.
Please click here to view our newest Virtual Networking video from Dr. Howard Goldberg of Howard Goldberg, MD, Inc.
Additional Virtual Networking videos from NEPHO providers can be found at here.
Please reach out to Alycia.Messelaar@lahey.org if you are interested in being featured in a Provider Spotlight or Virtual Networking video.
The Northeast PHO Provider Relations Department is excited to have you as part of our network of physicians!
In an effort to spread the word about the services you currently or will be providing, we would like to obtain information to be used to host virtual introductions, virtual drop-in sessions, a video to be posted on the NEPHO website, along with a provider spotlight bio to share with the NEPHO Primary Care Providers. Click here to be directed to our Virtual Networking page.
Please send requested marketing materials to Alycia Messelaar, Alycia.Messelaar@Lahey.org, in order to begin the marketing process.
Thank you,
The NEPHO Provider Relations Department
Please provide the following to create a 1-3 minute video about yourself. This can be done right from your smartphone! Please see Tips for Shooting better video on your smartphone.
Short bio (In paragraph format that includes the following information – please do not send a copy of your CV)
- Name
- Practice
- Specialty
- Ages treated
- Education/Training
- Past professional experience
- Special interests
- Whether you offer telehealth services
- Personal hobbies
- Professional photograph
- Best hours and days to set up brief virtual meetings with PCP practices that are interested in speaking with you directly
- Best ways to reach out directly regarding patient specific care questions
Please reach out to Alycia Messelaar, 978-236-1784 or Alycia.Messelaar@Lahey.org to keep NEPHO informed of changes in practice schedules due to COVID-19 (office closures, limited office hours, scope of appointment, telehealth use, phone line to reach staff, etc.) or if you have questions about other practice schedules.
Click here to access a list of practices who are scheduling in office visits and/or TeleHealth visits at this time. The PHO has discontinued sending the bi-weekly emails outlining this information. Please review your practice information and reach out to Alycia Messelaar, Alycia.Messelaar@Lahey.org with update requests. The updates will be included in this section in the next newsletter.
REFERRAL MANAGEMENT
The PHO Referral Management team is here to help with specialty referrals. As a reminder, referral requests outside of the Northeast PHO should be reviewed by our team. We have many new specialists in the Northeast PHO and we are learning more about the new specialists coming into the BILH network. We can help you find the appropriate provider to care for your patients.
Please send all out of PHO referral requests to our dedicated fax line at 978-236-1611. If you have any questions or need an urgent referral to a specialist, please contact Ann Cabral, Referral Manager at Ann.Cabral@Lahey.org or 978-236-1758.
PHARMACY
Please click on the following link to be redirected to the BILHPN May 2021 Newsletter:
BILHPN Newsletter Rx Cost Decision Tools/ Cost Saving Strategies/ Drug Coupons etc.
Update on Drug Coupons in Massachusetts
The Massachusetts Commercial Drug Coupon Program law was recently extended to 12/31/2022. The law mandates that drug coupons can only be used on drugs that do not have an AB rated generic approved by the FDA. Additionally, manufacturer drug coupons have implemented “newer language” in their individual Terms and Conditions of Use to reflect these requirements. Please see the 2021 May issue of the BILHPN Pharmacy Newsletter for more information.
Many pharmacies in Massachusetts are still not aware of the extension and are not accepting the coupons. If patients are denied they should alert their pharmacist about the extension to ensure the coupons are accepted. The citation is listed here: MA ST 175H § 3 (§ 3. Solicitation, improper inducement to use goods, facilities, services, or products covered by insurance).
Please keep in mind that the entire cost of the drug remains unchanged and is applied to total medical expense despite the reduced burden to the patient. As a reminder, high-cost drugs and use of drug coupons should be reserved for those patients in which a lower cost/generic alternative is not available and/or would not provide optimal clinical outcomes. Please continue to consider the most efficacious and cost-effective medications when determining the best pharmacotherapy option.
For more information or questions, please contact Carol Freedman, NEPHO Pharmacy Manager at
carol.freedman@lahey.org.
POPULATION HEALTH
On May 18, 2021 the United States Preventative Services Task Force (USPSTF) changed the recommendation for colorectal cancer screenings for adults at average risk. The USPSTF recommends that people at average risk begin screening for colorectal cancer at age 45. The new recommendation aligns with the American Cancer Society’s recommendation and is based on data which shows an increase in the incidence of colorectal cancer in younger adults.
The incidence of colorectal cancer, (specifically adenocarcinoma) in adults aged 40 to 49 years has increased by almost 15% from 2000-2002 to 2014-2016.¹ Currently colorectal cancer is the third leading cause of cancer death for both men and women. While colorectal cancer is most frequently diagnosed in persons aged 65 to 74 years, it is estimated that 10.5% of new cases occur in people younger than age 50.²
Certain groups may be more at risk for colorectal cancer. These groups include adults who identify as Black, Native American and Alaskan Native, people with a family history of colorectal cancer, men, as well as people with risk factors such as obesity, diabetes, long-term smoking and alcohol abuse.
Private insurance companies will now be required to cover colorectal cancer screening without cost-sharing starting at age 45 beginning in the plan year that begins on or after May 18, 2022 (one year from the latest issue date). Some plans may choose to cover the screening without cost-sharing earlier than the required date.
Below are the USPSTF Screening Interval Guidelines:
- High-sensitivity gFOBT or FIT every year
- sDNA-FIT every 1 to 3 years
- CT colonography every 5 years
- Flexible sigmoidoscopy every 5 years
- Flexible sigmoidoscopy every 10 years + FIT every year
- Colonoscopy screening every 10 years
- Montminy EM, Zhou M, Maniscalco L, et al. Contributions of adenocarcinoma and carcinoid tumors to early-onset colorectal cancer incidence rates in the United States. Ann Intern Med. 2021;174(2):157-166. Medline:33315473 doi:10.7326/M20-0068
- Siegel RL, Miller KD, Fedewa SA, et al. Colorectal cancer statistics, 2017. CA Cancer J Clin. 2017;67(3):177-193. Medline:28248415 doi:10.3322/caac.21395
QUALITY
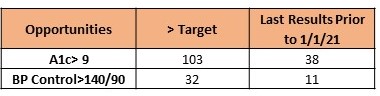
2021 Opportunities in Diabetes A1c and BP Control Measures
Quality performance in 2021 presents many challenges but opportunities for improving as well. The NEPHO’s 4 largest commercial contracts continue to emphasize “outcomes” measures, i.e. those measures which are results based as opposed to claims based. There are 3 outcomes measures:
- Diabetes A1c Control
- Diabetes BP Control
- Hypertension Controlling Blood Pressure (<140/90)
This article will identify opportunities for improved performance in the 2 Diabetes outcomes measures. According to the most recently received payer extracts for BCBS HMO & PPO, HPHC & THP, across the NEPHO there are 702 patients who have been identified as having diabetes and are in the Diabetes outcomes measures.
Harvard Pilgrim and Tufts Health Plan measure performance against the HEDIS 90th percentile. The HEDIS 90th percentile rates quality performance in relation to other organizations on a national level. Although the HEDIS performance threshold varies annually based on national performance rates, the performance thresholds would be similar to those for Blue Cross. Blue Cross HMO & PPO measure performance based on thresholds set by Blue Cross.
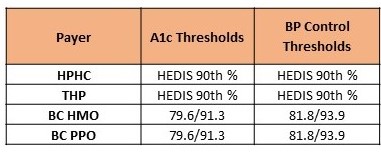
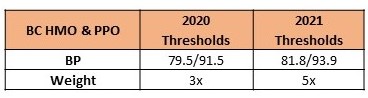
The Blue Cross minimum and maximum thresholds for the DM Blood Pressure Control measure increased slightly in 2021. Blue Cross also “weighs” the outcomes measures higher than the claims based process measures. As of 2021, Blue Cross outcomes measures will be weighted 5x the Blue Cross process measures. Combined with a decrease in the number of process measures from 19 to 8 for 2021, Blue Cross is increasing emphasis on results based measures rather than claims based measures.
The Northeast PHO strives to be among the top performers in the BILH Performance Network and BILH system in Quality. As always, it is challenging to meet the high thresholds set by the insurance plans but there are many opportunities for improvement.
- There are currently 103 patients whose last A1c was above the measure target (</=9.)
- Of those 103 patients, 38 have not yet had an A1c in 2021.
- Of these same 103 patients, 32 also have a last blood pressure reading above target (<140/90), 11 of which were taken prior to 1/1/21.
What will the NEPHO Quality Team do to help you meet our Quality goals?
- Our data analysts will work closely with your office manager and quality contacts to identify patients who need an appointment and/or labs.
- Our Nurse Case Managers will work directly with your patients to support them in managing their diabetes, encouraging adherence to medications and making healthier lifestyle choices.
- Our Population Health team will continue to identify quality care gaps for providers by entering pre-visit planning notes for diabetes patients with scheduled visits. The PVP pilot is with Epic practices only at this time with plans to expand to non-Epic practices in 2021.
What can you and your practice do to help optimize the NEPHO Quality performance in 2021? Below are some suggestions:
- Schedule an appointment for anyone who has not yet had a blood pressure reading in 2021. Patients with digital home blood pressure monitors may report their BP reading during a virtual visit with a provider.
- Order an HBA1c for any patient who does not yet have a result in 2021.
- Review diabetes related medications and attempt to establish a routine of regular follow up appointments for those patients with results above the targets for A1c and BP control.
- Take a second blood pressure if the first is 140/90 or greater.
Please contact anyone on the Quality Team with questions about the Diabetes outcomes or other Quality measures.
CODING TIP OF THE MONTH
OPTUM Newsletter – May 2021 | Chronic Kidney Disease
Risk Adjustment Hierarchical Condition Categories (HCC) Coding Examples
HCC coding capture will help create the patient Risk Adjustment Factor (RAF) score that will drive the future year allocation of resources to care for the patient. Making sure to capture a patients true health status is supported by ICD-10 CM coding capture. Highlighted are the top 10 HCC codes with coding examples to help support coding to the highest specificity.
- Diabetes without Complication (HCC 19)
- Example: Patient is seen in office for diabetes management. Diabetes is stable and patient working on nutrition improvement, exercise, stopped smoking and will continue seeing PCP every 3 months to support diabetes management.
- Code Diabetes Type II – E11.9
- Example: Patient is seen in office for diabetes management. Diabetes is stable and patient working on nutrition improvement, exercise, stopped smoking and will continue seeing PCP every 3 months to support diabetes management.
- Breast, Prostate, and Other Cancers and Tumors (HCC 12)
- Example: Patient is seeing PCP after prostate cancer treatment. The patient is stable, still seeing oncologist and on treatment with Flutamide. The prostate cancer is still being treated.
- Code Prostate Cancer – C61
- Example: Patient is seeing PCP after prostate cancer treatment. The patient is stable, still seeing oncologist and on treatment with Flutamide. The prostate cancer is still being treated.
- Diabetes with Chronic Complications (HCC 18)
- Example: Patient is coming in for 3 month check and has Diabetes Type II, Hypertension, CKD 3 stage 3a, and Morbid Obesity with BMI >40.
- Code Diabetes with CKD stage 3a – E11.22, N18.31, Diabetes with Complications E11.69, I10, E66.01, Z68.41, Hypertension with CKD E13.0
- Example: Patient is coming in for 3 month check and has Diabetes Type II, Hypertension, CKD 3 stage 3a, and Morbid Obesity with BMI >40.
- Seizure Disorders and Convulsions (HCC 79)
- Example: Patient was diagnosed 2 years ago with seizure disorder. The patient is still taking ethosuximide to manage condition but the provider did not document the condition last year. Patient is having Annual Wellness Visit (AWV) and the provider documented the seizure disorder is stable.
- Code Seizure Disorder – J40.909
- Example: Patient was diagnosed 2 years ago with seizure disorder. The patient is still taking ethosuximide to manage condition but the provider did not document the condition last year. Patient is having Annual Wellness Visit (AWV) and the provider documented the seizure disorder is stable.
- Specified Heart Arrhythmias (HCC 96)
- Example: Codes for Atrial Fibrillation (AF) types, these four unique codes describe the types of AF:
- Persistent AF (I48.11) describes AF that does not terminate within seven days, or that requires repeat pharmacological or electrical cardioversion.
- Permanent AF (I48.21) is persistent or longstanding persistent AF where cardioversion cannot or will not be performed, or is not indicated.
- Chronic AF, unspecified (I48.20) may refer to any persistent, longstanding persistent or permanent AF.
- Chronic persistent AF has no widely accepted clinical definition or meaning. Code I48.19, Other persistent atrial fibrillation, should be assigned.
- Example: Codes for Atrial Fibrillation (AF) types, these four unique codes describe the types of AF:
Documentation should include: In coding, “history of” indicates a condition is no longer active. Document in the note any current associated physical exam findings (such as irregular heart rhythm or increased heart rate) and related diagnostic testing results.
- Congestive Heart Failure (HCC 85)
- Example: A patient is seen for chronic diastolic heart failure and essential hypertension, the provider documents that both conditions are stable.
- Code I11.0 (hypertensive heart disease with heart failure), I50.32 (chronic diastolic heart failure), I10 (hypertension).
- Example: A patient is seen for chronic diastolic heart failure and essential hypertension, the provider documents that both conditions are stable.
- Other Significant Endocrine and Metabolic Disorders (HCC 23)
- Example: Patient is seen by provider for management of Diabetes II, the patient has hyperlipidemia, hypertension, CKD stage 3a, the patient is morbidly obese BMI >40.
- Code Diabetes with CKD 3 E11.22, N18.31, Diabetes with complications E11.69, E78.5, I10, E66.01, Z68.41
- Example: Patient is seen by provider for management of Diabetes II, the patient has hyperlipidemia, hypertension, CKD stage 3a, the patient is morbidly obese BMI >40.
- Chronic Obstructive Pulmonary Disease (HCC 111)
- Example: Patient is seen for 3 month follow-up visit for COPD with asthma and history of tobacco dependence. You don’t need a code for asthma since the type of asthma isn’t documented; you do need a code for history of tobacco dependence.
- Code J44.9, COPD, unspecified, Z87.891, personal history of nicotine dependence
- Example: Patient is seen for 3 month follow-up visit for COPD with asthma and history of tobacco dependence. You don’t need a code for asthma since the type of asthma isn’t documented; you do need a code for history of tobacco dependence.
- Major Depressive, Bipolar, and Paranoid Disorders (HCC 59)
- Example: The patient is a 35-year-old woman seeking weight loss surgery. She has struggled trying to lose weight; she states she has always been an overeater. Her spouse passed away October 2019 due to unexpected complications in the hospital. She was diagnosed with depression. Since then, she has been able to cope and feeling much better. She is calm and denies suicidal ideations. She denies tobacco use at this time but does have a history of smoking.
- Code F32.5 Major depressive disorder, single episode, in full remission, E66.01 Morbid (severe) obesity due to excess calories, Z68.42 Body mass index (BMI), 45.0-49.9, adult, Z87.891 Personal history of nicotine dependence.
- Example: The patient is a 35-year-old woman seeking weight loss surgery. She has struggled trying to lose weight; she states she has always been an overeater. Her spouse passed away October 2019 due to unexpected complications in the hospital. She was diagnosed with depression. Since then, she has been able to cope and feeling much better. She is calm and denies suicidal ideations. She denies tobacco use at this time but does have a history of smoking.
- Morbid Obesity (HCC 22)
- Example: The diagnosis of Morbid Obesity with a BMI of 40 or greater. If no BMI is documented, the diagnosis of Morbid Obesity will not be accepted as documented by the provider. The documentation of a BMI of 40 or greater is not accepted on face value to indicate a diagnosis of Morbid Obesity. The provider must document the clinical condition – Morbid Obesity.
- Code Morbid Obesity with BMI>40 to have coding risk adjust – Morbid Obesity E66.01, BMI>40 Z68.41.
- Example: The diagnosis of Morbid Obesity with a BMI of 40 or greater. If no BMI is documented, the diagnosis of Morbid Obesity will not be accepted as documented by the provider. The documentation of a BMI of 40 or greater is not accepted on face value to indicate a diagnosis of Morbid Obesity. The provider must document the clinical condition – Morbid Obesity.
Please contact Shawn Bromley at shawn.m.bromley@lahey.org or 978-236-1777 if you would like more detail regarding the importance of risk adjustment coding capture for outpatient services.
PATIENT EXPERIENCE COMMENTS
Blackburn Primary Care, Gloucester – 1 Blackburn Drive
- I love Dr. Jay Isaac, he is always kind, patient and takes the time I need during all appointments.
Lahey Primary Care, Beverly – 30 Tozer Road
- Dr. Susan Deluca always is so knowledgeable kind & patient. She is a great listener & doctor!
- Dr. Tina Waugh is an incredible diagnostician and is able to know me very well. She is always prompt and super caring.
Lahey Primary Care, Beverly – 900 Cummings Center
- Dr. Andrew Lendhardt is the most knowledgeable, patient and caring doctor. He is amazing.
Lahey Primary Care, Danvers – 5 Federal Street
- Dr. Mauri Cohen is the best physician. He is a shining star and example to his profession.
- Dr. Margaret Legner – This practice takes personal interest and wants to address your problems.
Lahey Primary Care, Danvers – 480 Maple Street
- Dr. Galina Feldman is great you never feel rushed. She listens to all your concerns.
Lahey Health Primary Care, Gloucester – 298 Washington Street 1st Floor
- Dr. Amy Esdale always seems interested and takes time to hear what I am concerned about.
Lahey Primary Care, Manchester (LPCO) – 192 School Street
- Dr. Jana Oettinger is an exceptional PCP providing extraordinary care through compassion, best practice care, wonderful communication and follow up.
North Shore Pediatrics, 480 Maple Street
- We always have a wonderful experience with Dr. Shannon Dufresne. She is amazing.
PRACTICE RECOGNITION
The Northeast PHO recognizes colleagues who provide a positive experience for our patients, help us keep care local and meet our quality targets.
This month’s winner is:
Ashley Nunes, Lahey Health Primary Care, Gloucester, was recognized for supporting quality improvement efforts for patients with diabetes and hypertension.

Ashely Nunes and Karen Damico, MD
Please let us know if you would like to nominate a team member in your practice or another practice for the recognition program. We will deliver gift cards to the winners each month, and they will be announced here and in our website “Hot Topics” section.