Outcomes Measures (A1c <9, DM BP Control <139/89 & HTN Control <139/89)
The 2023 BILHPN Ambulatory Quality Goal is to reach 85% compliance by December 31st in the 3 “outcomes” measures, i.e. those measures which are results based as opposed to claims based. There are 3 outcomes measures:
- Diabetes A1c Control
- Diabetes BP Control
- Hypertension Controlling Blood Pressure (<139/89)
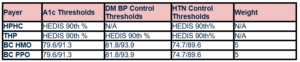
Harvard Pilgrim and Tufts Health Plan measure performance against the HEDIS 90th percentile (Healthcare Effectiveness Data and Information Set). The HEDIS 90th percentile rates quality performance in relation to other organizations on a national level. Performing at or above the 90th% puts organizations in the top 10% nationally. The HEDIS performance thresholds can vary annually based on national performance rates.
Blue Cross HMO & PPO measure performance based on thresholds set by Blue Cross. Blue Cross also applies “weights” to quality measures with the outcomes measures weighted 5x more than the process measures (cancer screenings, chlamydia screening, DM eye exam, etc.).
What will the NEPHO Quality Team do to help meet our Quality goals? Here are select examples:
- Our Population Health Specialist manages the Concierge Mammogram Scheduling Program, scheduling patients who are due for mammograms, following with reminder calls and following up cancelations or no shows.
- Our data analysts will work closely with your office manager and quality contacts to identify patients who need an appointment and/or labs by distributing regular Needs Appointment lists. We will continue to identify quality care gaps for providers by entering pre-visit planning notes for diabetes patients with scheduled visits, as well as applying appointment notes in Epic and registration notes in Centricity.
- Our Unhealthy BP Outreach Team will meet weekly to identify patients with gaps in care for the Hypertension Control Measure. The clinical members of the Team will work directly with your patients to support them in managing their hypertension, encouraging adherence to medications and making healthier lifestyle choices, as well as encouraging them to attend follow up appointments with PCP and specialists.
What can you and your practice do to help optimize the NEPHO Quality performance in 2023? Below are some suggestions:
- Schedule an appointment for anyone who has not had a blood pressure reading in 2023. Patients with digital home blood pressure monitors may report their BP reading during a virtual visit with a provider.
- Order an HBA1c for any patient who does not yet have a result in 2023.
- Review diabetes related medications and attempt to establish a routine of regular follow up appointments for those patients with results above the targets for A1c and BP control.
- Take a 2nd blood pressure if the first blood pressure is >139/89.
- Encourage your patient to obtain a home blood pressure monitor. Blood pressures taken at home tend to be more reflective of a patient’s true BP. The Quality Team has blood pressure monitors available to loan to patients. Please contact Elizabeth Isaac @ Elizabeth.isaac@lahey.org if you have a patient who would benefit from this program.
- Record home blood pressure readings in the medical record. Patient reported blood pressures may be submitted to the payers during settlement as long as the medical record reflects the date, time and actual systolic/diastolic reading.
Please contact anyone on the NEPHO Quality Team with questions about the Diabetes outcomes or other Quality measures.